An Evidence-Based Approach to Ultrasound Training
Learn how to maximize ultrasonography as a tool through compentency-based training. With simulation, learners can develop necessary psychomotor...
Today, physicians are challenged to develop skills that add value. Bedside ultrasound has been shown to better clinical diagnoses and manage patients.

Today’s complex healthcare work environment requires a multidisciplinary, team-based approach to patient care. Traditional tasks and roles formerly reserved for physicians are now being transitioned to advanced practice providers such as physician assistants, nurse practitioners, certified nurse midwives, clinical nurse specialists, and certified registered nurse anesthetists (Cooper et al.). There are approximately 248,000 nurse practitioners and 115,500 physician assistants in the United States (AANP, AAPA, PCE).
A typical medical school graduate that completes a primary care residency program will have undergone 13,500 to 15,000 more hours of clinical training, as compared to a nurse practitioner with a doctorate, before independently caring for patients (Sharma et al.). The challenge for educators is to ensure that the additional 10K+ hours of training medical students and residents undergo directly translates into valuable knowledge and enduring ultrasound skills that will lead to improved patient care.
The ability to precisely assess, evaluate, and manage patients is an essential core competency for today’s medical school graduates and will continue to be so in the future. Traditional methods of performing a physical examination are of critical importance. However, clinicians who perform a physical examination coupled with point-of-care ultrasound, a.k.a. bedside ultrasound, are uniquely empowered to better understand patient anatomy and detect pathologic conditions (Afonso et al., Angtuaco et al., Dreher et al., Mouratev et al.).
Introducing bedside ultrasound applications as a supplement to learning standard physical examination principles reinforces both processes. This combined approach enables students to visualize underlying patient anatomy and pathologic findings in real time rather than relying upon illustrations. In an ultrasound-based clinical initiative from the University of California, Irvine, Fox et. al. insightfully built upon the original Stanford 25 physical examination (Kugler and Verghese). Fox and colleagues described ultrasonographic examinations that directly complement standard physical examination techniques and named this augmented patient exam the “UCI 30.”
Bedside ultrasound has been shown to improve medical student knowledge of human anatomy and physiology (Afonso et al., Brackney et al., Griksaitis et al., Ivanusic et al., Parikh et al., Shapiro et al., Steinmetz et al., Teichgräber et al., Wittich et al.). In fact, ultrasound can help trained operators better establish clinical diagnoses and manage patients (Butter et al., Decara et al., Patel et al., Tshibwabwa et al., Wittich et al.).
Bedside ultrasound has hundreds of applications across multiple specialties, positively affecting the lives of millions globally. Applications include identifying high-risk pregnancies such as breech presentations, decreasing the number of needle sticks and time it takes to establish intravenous access, and identifying life-threatening abdominal aneurysms at risk for imminent rupture. The range of clinical applications for which bedside ultrasound is being used is rapidly expanding.
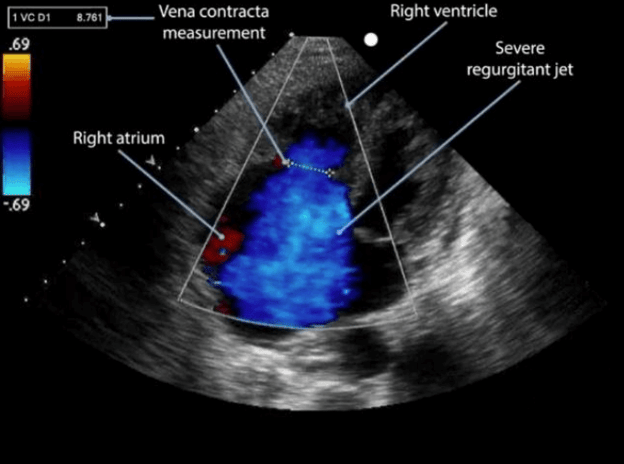 Severe Tricuspid Regurgitation (Color Doppler)
Severe Tricuspid Regurgitation (Color Doppler)
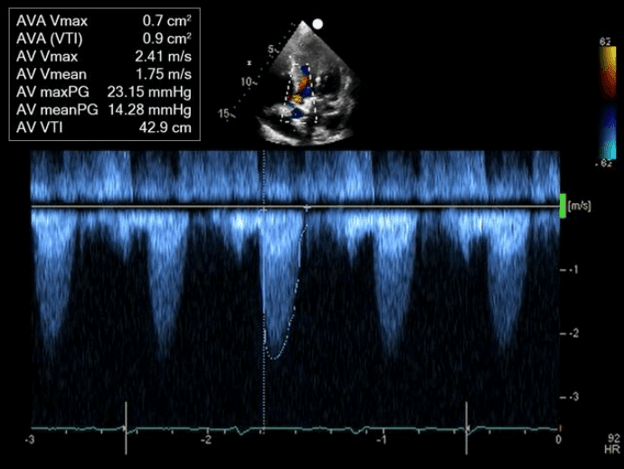 Aortic Stenosis (Spectral Doppler Waveforms)
Aortic Stenosis (Spectral Doppler Waveforms)
Cardiac conditions such as valvular and nonvalvular disorders that are inferred by auscultation can be visualized and precisely quantified with cardiac ultrasound a.k.a. termed echocardiography (Kimura et al., Kobal et al.). In a dramatic study, Kobal et al. demonstrated that the diagnostic accuracy of first-year medical students with 18 hours of ultrasound education was superior to board-certified cardiologists performing a cardiac physical examination for the detection of valvular and nonvalvular cardiac abnormalities. Medical students correctly identified 75% (180 of 239) of pathologic conditions, while the cardiologists identified only 49% (116 of 239) (p <0.001).
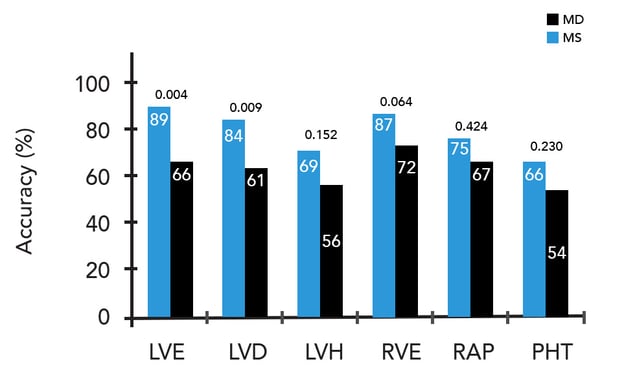 Medical student (MS) and cardiologist (MD) diagnostic accuracy for nonvalvular lesions. LVD = LV dysfunction; LVE= LV enlargement; LVH= LV hypertrophy; RAP= right atrial pressure; RVE= right ventricular enlargement; PHT= pulmonary hypertension
Medical student (MS) and cardiologist (MD) diagnostic accuracy for nonvalvular lesions. LVD = LV dysfunction; LVE= LV enlargement; LVH= LV hypertrophy; RAP= right atrial pressure; RVE= right ventricular enlargement; PHT= pulmonary hypertension
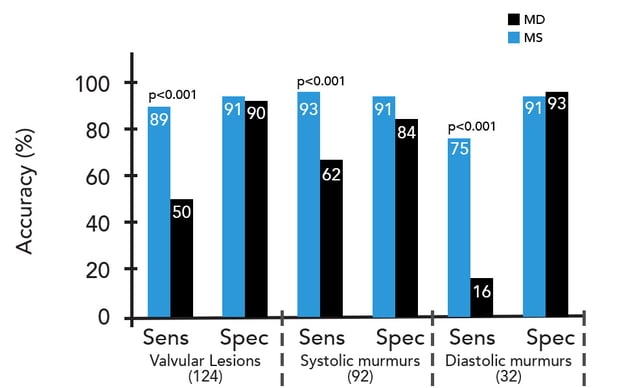 Medical students’ and cardiologists’ (MD) diagnostic sensitivity (sens) and specificity (spec) for valvular lesions
Medical students’ and cardiologists’ (MD) diagnostic sensitivity (sens) and specificity (spec) for valvular lesions
Adapted from: Kobal SL, Trento L, Baharami S, et al. Comparison of the effectiveness of hand-carried ultrasound to bedside cardiovascular physical examination. Am J Cardiol. 2005 Oct 1;96(7):1002-6. doi: 10.1016/j.amjcard.2005.05.060. PMID: 16188532.
Time-sensitive definitive diagnoses, such as a ruptured abdominal aortic aneurysm, are now achieved with bedside ultrasound in minutes rather than hours (Plummer et al., Tayal 2003 et al.). The differential diagnosis of undifferentiated shock is narrowed in minutes using bedside ultrasound. Clinicians may use it to evaluate cardiac ejection fraction, exclude tension pneumothorax, noninvasively estimate central venous pressures by visualizing respirophasic variation in inferior vena cava diameter, assess for right heart overload or pericardial effusion, and screen for intracorporal blood loss in major body cavities (Gunst et al., Madill et al., Melniker et al., Nagdev et al., Rozycki et al., Salen et al.).
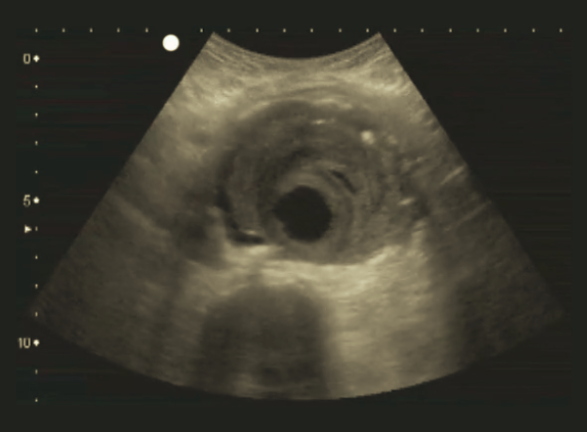 Abdominal Aortic Aneurysm With Mural Thrombus
Abdominal Aortic Aneurysm With Mural Thrombus
Possessing the ability to establish peripheral venous access in a “difficult-stick patient” is a must-have skill for medical students. Blind, landmark-based techniques may prove difficult in some patients due to anatomic variations, or veins that may be scarred from previous indwelling catheters or blood specimen phlebotomy. There are also patients for whom obtaining vascular access may be difficult due to a transient medical situation, such as low blood volume or shock. In these cases, a delay in obtaining vascular access may prolong diagnosis and treatment, thereby endangering the patient.
Medical school graduates that know how to utilize ultrasound to help guide the insertion of peripheral intravenous catheters will mitigate delays in administering therapeutic agents, reduce complications from multiple unsuccessful needle sticks, and decrease the time needed to ascertain diagnoses. Using ultrasound for peripheral intravenous catheter insertion has been shown to lessen patient pain and anxiety, and improve overall patient experience (AHRQ, Bahl et al., Oliveira & Lawrence, Lamperti et al., Moore et al.).
 Insertion of a Peripheral Intravenous Catheter using In-Plane Needle Guidance. (2D Ultrasound)
Insertion of a Peripheral Intravenous Catheter using In-Plane Needle Guidance. (2D Ultrasound)
A subset of critically ill patients will require central venous catheter placement. Blind, landmark-based central venous catheter placement is unsuccessful in 20 percent of attempts. Performing this procedure without the use of ultrasound also has an associated 10 percent minor and major complication rate, and such complications may include arterial puncture, iatrogenic pneumothorax, hemothorax, air embolus, arrhythmias, catheter knotting, hemothorax, chylothorax, and brachial plexus injury (AHRQ). Ultrasound guidance is a documented method of decreasing central venous line placement complications by 78 percent (AHRQ, NICE, Bansal et al., Miller AH et al.).
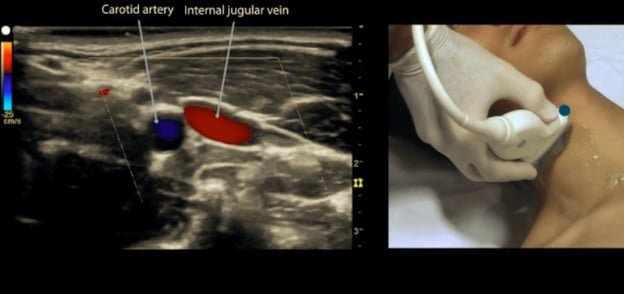 Internal Jugular Vein & Carotid Artery (Color Doppler Ultrasound)
Internal Jugular Vein & Carotid Artery (Color Doppler Ultrasound)
Given the many benefits of bedside ultrasound, medical schools across North America have integrated ultrasound into their curricula, and medical students worldwide have recognized its value. They organize medical ultrasound interest groups and serve as catalysts for integrating ultrasound training into their respective institutions (Celebi et al., Chiem et al., Coiffier et al., Wilson et al.).
Medical schools have begun to incorporate bedside ultrasound in a variety of ways. Focused ultrasound instruction has been utilized as an adjunct to teaching human anatomy, performing a physical examination, and executing needle-based procedures (Afonso et al., Brackney et al., Griksaitis et al., Hoyer et al., Ivanusic et al., Nelson et al., Shapiro et al., Teichgräber et al., Wittich et al.). Certain institutions have committed to a more comprehensive integration of ultrasound instruction across all four years of medical school (Bahner et al., Hoppmann et al., Miller GT et al., Wilson et al., Rao et al.).
Despite the introduction of ultrasound into clinical medicine in 1942, widespread adoption of the imaging modality in patient care has not yet occurred due to training challenges (Shampo & Kyle). Historical barriers to ultrasound training include the need for an ultrasound machine, a patient with a relevant pathologic condition, a qualified instructor, a teaching moment, and the ability to repeat this process until mastery (Figure 1). Each of these elements must be available for every particular ultrasound application if a learner wishes to achieve a high level of proficiency. Recent improvements in machine performance reduced production costs, and the miniaturization of ultrasound machines have made ultrasound education and training the “last remaining hurdle” to the widespread adoption of bedside ultrasonography and the realization of its benefits.
|
Barriers to Ultrasound Instruction |
Barriers to Ultrasound Curriculum Integration |
|
Ultrasound machine |
Lack of funding for machines & maintenance |
|
Qualified instructor |
Limited faculty time for instruction |
|
Patient with pathology |
Restricted clinical access to patients |
|
A teaching moment |
An overfilled medical school curriculum |
|
Refresher training |
Lack of resources for assessment |
Figure 1.
Recent studies conducted by Bahner et al. and Dinh et al. describe the commonly faced challenges in integrating ultrasound training into medical education. Lack of funding, training resources, and space within existing curricula are cited as major obstacles. Additional barriers to ultrasound training during clinical rotations include providing medical students with sufficient access to ultrasound machines and having patients readily available with specific pathologic conditions that correlate to didactic instruction. Finally, the resources required to assess competency, track performance, provide feedback, and archive performance metrics are often underestimated by instructors.
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) pandemic has had a devastating impact on medical education. The coronavirus pandemic lockdowns and continued fear of COVID-19 transmission have created many additional barriers to ultrasound education, most notably, by cutting off an entire generation of ultrasound learners from accessing clinical training sites. Ultrasound learners, including medical students and residents alike, lost the critical component of access to bedside ultrasound training within clinical settings.
According to the American College of Emergency Physicians, “The training process for ultrasonography should include didactic and practical hands-on training. It must also include experiential and competency components”. Effective ultrasound training includes the speed of image acquisition, target structure acquisition (image view), and diagnostic interpretation. These elements are subsequently linked to a performance review and improvement process.
The conventional method for teaching medical procedures involves a “see one, do one, teach one” approach (Vozenilek et al.). This historical approach does not overcome the previously described barriers and fails to provide a pathway for large-scale implementation of ultrasound training. It is also progressively becoming less acceptable to expose patients to the potential risk of complications for the sake of novice trainee instruction in all areas of medicine.
The advent of the COVID-19 pandemic has accelerated the need for training institutions to build in the flexibility to support remote instruction (Gottlieb et al.). Fortunately, recent advances in web-based education and ultrasound simulation technologies have provided new education and training pathways (Gottlieb et al., Liteplo et al., Tayal 2018 et al.).
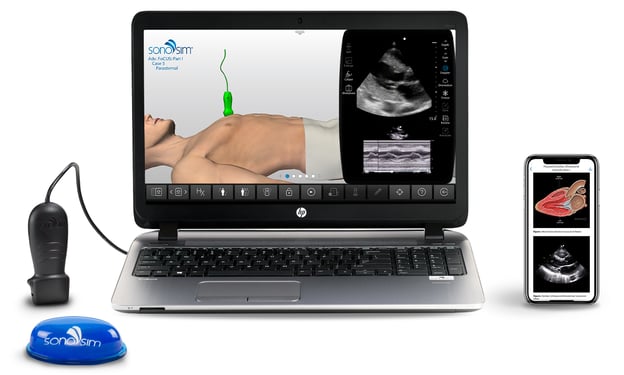 SonoSim Ultrasound Training delivers cloud-based didactic instruction, image acquisition, and interpretation assistance, hands-on training, performance tracking, and automated assessment powered by AI
SonoSim Ultrasound Training delivers cloud-based didactic instruction, image acquisition, and interpretation assistance, hands-on training, performance tracking, and automated assessment powered by AI
Innovative ultrasound training is meeting the need for scalable ultrasound education. Medical students can now access didactic ultrasound instruction via courses on mobile apps and acquire ultrasound image acquisition (scanning) and interpretation skills through proven, validated ultrasound training (Adhikari et al., Azizi et al., Chung 2011 et al., Chung 2013 et al., Iseli & Savitsky 2015, Iseli et al. 2016, Iseli et al. 2019, Maw et al., Miller GT et al., Monti et al., Paddock et al., Rebel et al., Rowley et al.).
Trainees can learn how to apply ultrasound findings toward medical decision-making and practice ultrasound-guided procedures in a risk-free environment using cognitive task training modules. Learners can access an online virtual tutor anytime and get real-time image acquisition and interpretation feedback powered by artificial intelligence (AI).
Medical professionals and educators can leverage blended learning ultrasound education that complements clinical ultrasound education. Elements include remote didactic instruction, virtual hands-on ultrasound technology training, and automated assessment using AI. These validated tools can help ultrasound educators deliver cost-effective, standardized ultrasound education in a scalable manner. The integration of bedside ultrasound into undergraduate medical education provides medical students with valuable anatomic knowledge and instills an enduring, high-level skill set for enhanced patient care.
Learn how to maximize ultrasonography as a tool through compentency-based training. With simulation, learners can develop necessary psychomotor...
Learn how SonoSim responds to AIUM's new OBGYN ultrasound training recommendations by providing residency programs with competency-based learning...
Using simulation technologies, learn how gamification and competitions are increasing interest among medical students in learning ultrasonography.
Get the latest trends in ultrasound training, education, & applications delivered to your inbox.
Have Questions?
Click here to chat!