A National Point-of-Care Ultrasound Competition for Medical Students
Using simulation technologies, learn how gamification and competitions are increasing interest among medical students in learning ultrasonography.
Learn how to maximize ultrasonography as a tool through compentency-based training. With simulation, learners can develop necessary psychomotor skills.

In 1999, the American Medical Association (AMA) affirmed that ultrasound imaging was within the scope of practice for appropriately trained physicians and acknowledged the broad and diverse applications of ultrasound within the medical field. Since then, bedside ultrasound has enjoyed tremendous growth across multiple medical specialties. Ultrasound training is commonplace in Emergency Medicine, Critical Care ultrasound, Obstetrics and Gynecology, Radiology, Internal Medicine, Family Medicine, General Surgery, and Pediatrics residency programs and clinical practice across the United States.
Medical students will experience firsthand the central role ultrasound plays in daily patient care ultrasound during their clinical clerkships. As a result, today’s medical students are progressively advocating for the greater integration of ultrasound into undergraduate medical education. Multiple studies have demonstrated that bedside ultrasound is shown to improve medical students’ knowledge of human anatomy and physiology (Afonso et al., Brackney et al., Butter et al., Decara et al., Griksaitis et al., Ivanusic et al., Parikh et al., Patel et al., Shapiro et al., Steinmetz et al., Teichgräber et al., Tshibwabwa et al., Wittich et al.). Bedside ultrasound is a well-established method of improving clinicians’ ability to rapidly diagnose and manage patients. Evidence supporting the clinical impact of bedside ultrasound, coupled with fervent interest from students, has led to the progressive integration of clinical ultrasound training courses into undergraduate medical education.
Medical school leaders seeking to implement ultrasound training at their institutions understand that similar to a stethoscope, ultrasound is an operator-dependent modality. Ultrasound is only as useful as the user’s ability to obtain an ultrasound image, interpret it, and apply the findings to medical care. One of the first tasks facing medical ultrasound educators is defining the breadth and depth of ultrasound education.
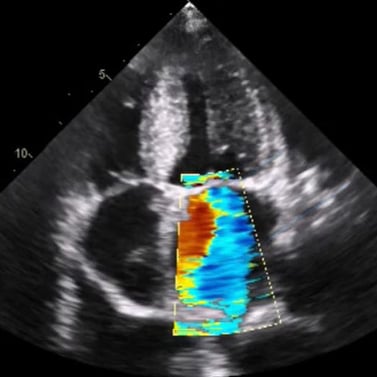 Color Doppler Ultrasound of Mitral Valve (Apical, Four-Chamber View)
Color Doppler Ultrasound of Mitral Valve (Apical, Four-Chamber View)
Ultrasound is only as useful as the user’s ability to obtain an ultrasound image, interpret it, and apply the findings to medical care.
The American Institute of Ultrasound in Medicine (AIUM) is a multidisciplinary association dedicated “to advancing the safe and effective use of ultrasound in medicine through professional and public education, research, development of guidelines, and accreditation.” The AIUM cites five fundamental principles of ultrasound physics and instrumentation that are essential to optimizing diagnostic images and patient safety. These include the ability to:
Mastery of these fundamental principles will provide medical students with a solid foundation for future ultrasound learning. Fortunately, medical professionals seeking to expand the role of ultrasound within their institutions can leverage the published experiences of medical schools that have already incorporated bedside ultrasound. Focused ultrasound instruction has been utilized by medical school educators as an adjunct to teaching human anatomy, performing a physical examination, and executing needle-based procedures (Afonso et al., Brackney et al., Griksaitis et al., Hoyer et al., Ivanusic et al., Nelson et al., Shapiro et al., Teichgräber et al., Wittich et al.). Some institutions have committed to a more comprehensive integration of ultrasound instruction across all four years of medical school (Bahner et al., Hoppmann et al., Miller GT et al., Wilson et al., Rao et al.).
Once an ultrasound curriculum is defined, medical leaders are faced with the task of deciding what constitutes ultrasound competency at their respective institutions. In 2013, a consensus agreement regarding the elements required to demonstrate ultrasound competency on specific ultrasound applications was achieved and published by Tolsgaard et al. Ultrasound competency is defined by demonstrating an understanding of the indications for an ultrasound examination, applied knowledge of ultrasound equipment, image optimization skills, the ability to independently perform a systematic ultrasound examination, interpret images, document the examination, and apply the findings towards medical decision making.
Elements of Ultrasound Competency
|
Indication for the examination |
Interpretation of images |
|
Applied knowledge of ultrasound equipment |
Documentation of examination |
|
Image optimization |
Medical decision making |
|
Systematic examination |
|
Adapted from: Tolsgaard MG, Todsen T, Sorensen JL, et al. International Multispecialty Consensus on How to Evaluate Ultrasound Competence: A Delphi Consensus Survey. Milanese S, ed. PLoS ONE. 2013;8(2):e57687. doi:10.1371/journal.pone.0057687.
Beyond defining the elements that constitute ultrasound competency for selected ultrasound applications, a precise understanding of the knowledge, skills, and attributes (KSA) that contribute to achieving it is important. A combination of declarative knowledge on a particular ultrasound application (such as the use of ultrasound for evaluation of biliary colic) and procedural knowledge (such as the ability to perform a gallbladder and biliary tree ultrasound examination) is required to successfully evaluate a patient with bedside ultrasound. Each ultrasound application would ideally be taught in an evidence-based, standardized format consistent with the agreed-upon determinants of ultrasound competence.
A novice learner seeking to achieve competency on a chosen ultrasound application will need to receive didactic instruction on the topic; develop the psychomotor skills required to obtain the requisite ultrasound image and correctly interpret it, and develop the ability to take ultrasound findings and apply them towards medical decision making. Achieving ultrasound competency in a particular application is not a linear process. It involves applying recently acquired knowledge and skills towards clinical applications, appreciating which elements have been mastered, and acknowledging which ones require further reinforcement. Over time, novice learners will master the intended ultrasound application and can devote attention to broadening their ultrasound skill set.
Determining ultrasound competency entails establishing desired performance parameters and metrics of success. Performance parameters will vary based on the level of trainee, diagnostic application, and/or ultrasound-guided procedure. Competency assessment typically consists of a test of knowledge regarding the ultrasound application and the ability to execute the procedure. Assessment of cognitive knowledge is generally approached through written or oral examinations. There is evidence to indicate that interspersed questions and feedback during instruction correlate with better knowledge retention (Weinstock et al.).
Assessing manual skill competency is typically performed by direct human observation and retrospective review of saved ultrasound images/clips, and is often supplemented by simulation. This traditional approach to establishing ultrasound competency requires that a supervising ultrasound educator monitors learner performance across specified ultrasound applications and will decide when a learner has achieved sufficient knowledge and skill to perform the task independently (Lucas et al.). Many times, this process is rather informal and prone to subjectivity. Several studies have advocated for the use of performance checklists as a means of standardizing the process and improving interrater reliability of performance assessment (Lenchus et al., Walzak et al.).
Advances in ultrasound simulation now allow for real-time automated performance assessment on a variety of ultrasound tasks powered by artificial intelligence (Iseli et al., Lenchus et al., Millington et al., Walzak et al.). This creates a pathway for standardized assessment of large numbers of ultrasound learners.
The emergence of simulation-based ultrasound training solutions has provided a pathway to support ultrasound training and performance assessment (Iseli et al., Walzak et al.). Simulation provides an opportunity for learners to engage in deliberate practice within an environment that is safe for learners and patients alike (AIUM). Simulation can also accelerate learning curves and help programs increase the scale of training efforts in a standardized manner.
Medical educators must ensure that the selected simulation tools are capable of achieving desired outcomes. Stunt et al. reviewed 435 commercially available simulators that were marketed as methods for improving medical psychomotor skills training. They found that only 6% of these simulators were accompanied by validation studies demonstrating an improvement in medical psychomotor skills following the use of the products. Simulation-based training should be accompanied by direct observation in a clinical setting along the pathway to establishing competency (AIUM).
Successful performance of an ultrasound task is the best indicator of competency. However, when individuals fail to achieve success, an understanding of the specific elements that led to failure will enable constructive feedback. The ability to provide feedback on deficiencies in declarative knowledge, procedural knowledge, or psychomotor skill is beneficial. Selecting validated metrics that are predictive of competency is important (Iseli et al.). The declarative and procedural knowledge elements required for ultrasound competency for many ultrasound applications are well-understood. The challenge for medical educators quickly becomes amassing the resources such as time, funding, and effort that are required to create robust competency assessment processes.
 Validated Ultrasound Training Solutions Are Supporting Medical Training Institutions
Validated Ultrasound Training Solutions Are Supporting Medical Training Institutions
Validated and proven-effective ultrasound training and performance tracking solutions have been brought to market across a variety of ultrasound applications that can support such efforts (Adhikari et al., Azizi et al., Chung 2011 et al., Chung 2013 et al., Damp et al., Iseli 2019 et al., Iseli & Savitsky, Miller et al., Monti et al., Paddock et al., Rowley et al., Sommer et al., Tayal et al.).
The exact role psychomotor skills play in ultrasound competency remains to be defined (AIUM, Chapman et al., Iseli & Savitsky). Nicholls et al. defined psychomotor skills in the domain of medical ultrasound imaging as, “the unique mental and motor activities required to execute a manual task safely and efficiently for each clinical situation.”
Ultrasound-related psychomotor skills have been subdivided into visuomotor and visuospatial skills. Visuomotor skills, or hand-eye coordination, refer to the coordination of visual inputs and limb motor movements that are used to manipulate an ultrasound transducer to acquire the desired optimal image. Visuospatial skills have been defined as “the ability to perceive, comprehend, and conceptualize visual representations and spatial relationships” (Mosby, American Heritage). When assessing ultrasound performance, visuospatial skills have been characterized as the ability to mentally recreate three-dimensional anatomy from two-dimensional image slices and understand spatial relationships and orientation of objects (for example, needle tip relation to a target vessel) within regions of interest.
Iseli and Savitsky described findings regarding psychomotor skill development as part of a study seeking to validate a platform for use in ultrasound competency testing. They explored the relationship between a participant’s prior ultrasound experience and psychomotor skills. Ultrasound-related psychomotor skills were accessed by 59 study participants, ranging from novices with no prior ultrasound experience or training to sonographers with over 20 years of ultrasound experience. They found that prior ultrasound experience did not predict higher levels of intrinsic psychomotor skill. More experienced ultrasonographers performed worse on objective visuospatial testing. Moreover, they also found that psychomotor skill tends to diminish with age, which matched findings from prior studies in other domains. Younger, less ultrasound-experienced participants demonstrated superior psychomotor skills.
These study findings underscore the value of differentiating psychomotor “traits” from “skills.” A psychomotor ability or “trait,” is nonmodifiable and intrinsic to an individual, while a psychomotor “skill,” is modifiable with repetition and is task-specific. A better understanding of the relative contributions of intrinsic psychomotor traits versus trainable psychomotor skills will inform future ultrasound training and assessment efforts. Interim evidence indicates that medical students have age on their side and can be nurtured to achieve ultrasound skills.
Though scientific literature on skill decay is limited, it suggests that mastery of complex skills degrades over several months. Cognitive aspects of complex skills appear to degrade first with notable degradation occurring approximately three to six months after training. Psychomotor elements persist longer but will eventually degrade as well, with notable decay occurring after 10 to 12 months (Arthur et al 1998., Arthur et al 2007., Driskell et al., Wisher et al.). Critically, one of the first cognitive skills to show signs of degradation is the ability to prioritize and execute actions and responses in the appropriate order (Wisher et al.).
Refresher training is recommended to ameliorate skill decay and improve overall skill retention. Issues related to skill decay and the need for refresher training for ultrasound skill maintenance are highly relevant to graduate medical education and hospital credentialing bodies. They are of equal importance to medical school educators that are focused on creating a foundation of ultrasound knowledge and skills for their students. Further research is required to better define skill decay curves and refresher training intervals across ultrasound applications
 Laptop & Cloud Based Ultrasound Training from SonoSim
Laptop & Cloud Based Ultrasound Training from SonoSim
Medical school leaders are well aware that today’s learners prefer independent, on-demand access to learning resources delivered across a variety of platforms such as laptops, tablets, and smartphones. Medical students demand engaging, interactive educational experiences in place of traditional “textbook-based” instruction. Fortunately, medical educators can leverage proven-effective cloud-based ultrasound training solutions to develop declarative knowledge, and procedural knowledge, and provide medical students with real-time performance guidance, feedback, and competency assessment.
Using simulation technologies, learn how gamification and competitions are increasing interest among medical students in learning ultrasonography.
Point-of-Care ultrasound provides a unique opportunity for educators to pivot from time-based to competency-based learning while improving patient...
Learn how SonoSim responds to AIUM's new OBGYN ultrasound training recommendations by providing residency programs with competency-based learning...
Get the latest trends in ultrasound training, education, & applications delivered to your inbox.
Have Questions?
Click here to chat!